MBBS, MRCS(EDIN), MMED(SURG), FRCS(UROL) (RCPSG), FAMS(UROL)

BSC(Monash), MBBS(NSW), FRCS(Glasgow), FRACS, MMED(Surgery), FAMS(Urol)
Prostate cancer is one of the most common cancers affecting men, yet screening is often only
considered when symptoms appear or after a friend or family member is diagnosed. In reality,
prostate cancer frequently develops quietly, with early stages causing little to no noticeable
change. This is where prostate cancer screening plays an important role. By assessing your risk
before symptoms arise, screening allows for timely evaluation and more informed health decisions.
In this guide, we explain what prostate cancer screening involves, and what to expect at each stage.
Keep reading to see how screening fits into a proactive, long-term approach to men’s health.
What Is Prostate Cancer?
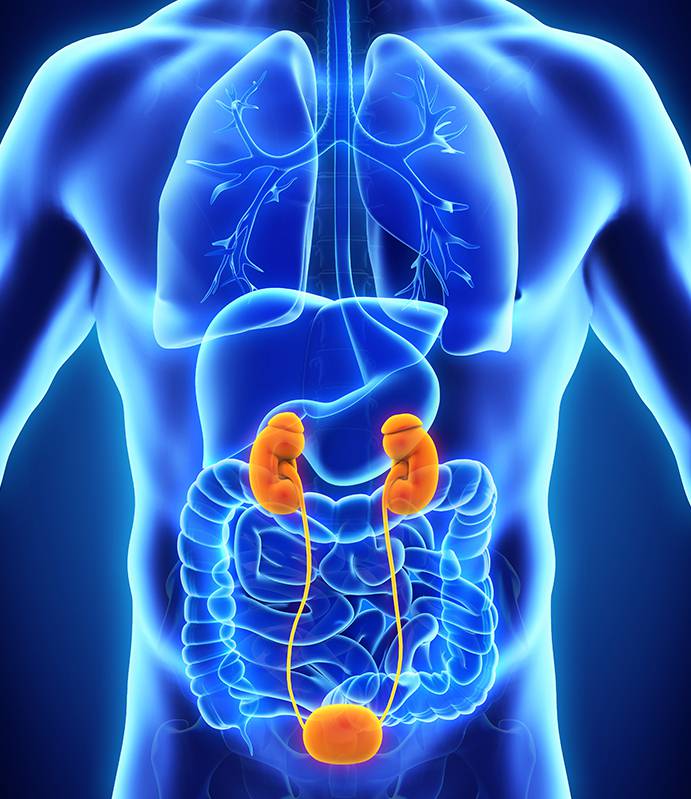
Prostate cancer develops when abnormal cells grow and multiply within the prostate gland. The prostate is a small, walnut-sized gland located just below the bladder, and it plays a key role in producing fluid that supports and transports sperm.
Most prostate cancers are adenocarcinomas, arising from the glandular tissue. Importantly, prostate cancer does not behave the same way in everyone. Some cancers grow very slowly and may never cause symptoms, while others are more aggressive and require prompt treatment. This variation is why discussing screening with a prostate cancer doctor at the appropriate age allows your care to be tailored to your individual risk profile.
Why Is Screening Important?
Screening is a proactive step that can significantly influence how prostate cancer is managed. By identifying changes early, doctors are better able to guide treatment decisions and long-term monitoring. Key benefits of screening include:
- Early Detection: Identifying prostate cancer when it is still localised offers the highest likelihood of successful treatment, often before symptoms develop.
- Accurate Monitoring: For men with low-risk disease, regular screening supports precise monitoring. This helps clinicians determine whether active surveillance remains appropriate or if treatment should be initiated.
- Improved Survival: International evidence shows that structured screening programmes reduce prostate cancer mortality by detecting the disease when it is more responsive to treatment.
- Informed Decision-Making: Screening provides objective clinical information, enabling patients and healthcare teams to make well-guided decisions that align with individual health needs and circumstances.
Who Should Consider Prostate Cancer Screening?
The decision to begin screening is personal and should be guided by your individual risk factors, including age, family history and ethnic background. A consultation with a prostate cancer specialist is the best way to determine a suitable screening plan. Screening discussions are generally recommended for:
- Men Aged 50 and Above: Men with an average risk profile are usually advised to begin discussing screening around age 50.
- Men with a Strong Family History: Those with a first-degree relative diagnosed before age 65 have an elevated risk and should consider discussing screening typically from ages 40 to 45.
- Men with Known Genetic Factors: Individuals carrying mutations such as BRCA1 or BRCA2 are at higher risk and should seek specialist advice early.
Preparing for a Prostate Cancer Screening
A little preparation before your appointment can help ensure more reliable results. Your doctor may advise you to:
- Avoid ejaculation, anal sex and vigorous exercise for 48 hours before a PSA test, as these can temporarily raise PSA levels
- Eat and drink as usual, as fasting is not required
- Inform your doctor about any urinary or rectal symptoms, including haemorrhoids, particularly before a digital rectal examination
- Prepare a list of current medications and supplements, and consider having a partner or family member accompany you for support
What to Expect During Screening
Prostate cancer screening typically involves one or both of the following assessments, used together to provide a clearer picture of prostate health.
PSA Blood Test
The prostate-specific antigen (PSA) test is a straightforward blood test performed at a clinic or laboratory. It takes only a few minutes, with a small blood sample collected to measure PSA levels. The results help determine whether further evaluation is needed.
Digital Rectal Examination (DRE)
Some men may also undergo a digital rectal examination. During this brief procedure, the doctor gently inserts a gloved, lubricated finger into the rectum to feel the back surface of the prostate. This allows the doctor to check for firmness, lumps or irregularities. While it may feel slightly uncomfortable, it should not be painful.
After the Screening: Understanding Your Results
Receiving your screening results is an important part of the process, and understanding what they mean can help you understand your next steps.
PSA Results
PSA results are usually available within one to two weeks. A level below 4 ng/mL is often considered within the normal range, though this varies with age, prostate size and overall health. An elevated PSA does not necessarily indicate cancer, as benign conditions such as prostate enlargement (BPH), inflammation or infection can also raise PSA levels.
Further Assessment if Needed
In the event your PSA remains elevated or if a DRE reveals any irregularities, your doctor may recommend additional assessments. These may include:
- A repeat PSA test
- MRI of the prostate
- A prostate biopsy
If a biopsy is performed, the results will include a Gleason score, which indicates how aggressive the cancer cells appear. Your specialist will explain what this means and discuss management options based on your individual risk.
Taking the Next Step in Prostate Health
Choosing to undergo prostate cancer screening is an important step towards proactive health management rather than waiting for symptoms to appear.
A qualified urologist is best placed to assess your PSA results, family history and personal health profile, as well as to design a screening plan suited to your needs. If you are considering prostate cancer screening or would like personalised advice, contact our team to arrange a consultation and discuss the next steps in caring for your health.

Dr Robert Tan Tin Kiat
Dr Robert Tan is a consultant urologist with more than 35 years of clinical experience. He began his career at Tan Tock Seng Hospital, where he was involved in the early use of Transurethral Resection of the Prostate (TURP), a procedure that continues to be widely used for the management of BPH. Since 1984 he has been in private practice at Gleneagles Hospital, caring for a broad range of patients over the years. Dr Tan is also one of the founding members of the Singapore Urological Association.

Dr Lincoln Tan
Dr Lincoln Tan is a consultant urologist and accredited robotic surgeon practising at Mount Elizabeth Hospital. Before joining Tan Urology, he served as director of Urologic Oncology at the National University Hospital and the National Cancer Institute of Singapore, where he continues as a visiting consultant. He is trained across the full spectrum of urology, with a focus on minimally invasive techniques, including laparoscopic and robotic-assisted surgery for prostate and kidney cancers.