Diagnosing and Treating Testicular Cancer
How common is testicular cancer?
While testicular cancer overall is an uncommon cancer, it is the most common solid tumour in young men between the ages of 15 and 40 years. All young men should regularly do self-examination of their testicles.

What are the risk factors for testicular cancer?
The exact causes are unknown but there are a few risk factors for testicular cancer.
History of undescended testis:
- An undescended testis has a 3% - 5% chance of developing testicular cancer, with the risk increasing the higher the testis location.
- Previous testicular cancer in the other testis.
- Family history of testicular cancer (father or brother).
- Poorly developed testes associated with an intersex disorder.
What are the signs and symptoms of testicular cancer?
Common symptoms of include:
- A painless lump or swelling in your testicle
- Back pain from the spread of testicular cancer to the abdomen (retroperitoneum)
- Breast swelling or enlargement (uncommon)
- A sensation of heaviness in the scrotum
- Pain or discomfort in the scrotum or testicle
In most cases, only one testicle is affected; about 1% - 3% of cancers occur in both testicles.

What tests are needed to diagnose testicular cancer?
A scrotal ultrasound is the most important test to visualise a tumour. In most cases, it can differentiate testicular cancer from other causes of testicular swelling. If you are experiencing symptoms of testicular cancer, the following tests may be required:
Blood tests:
- Tumour markers (AFP, HCG, LDH) are helpful in determining what type of testicular cancer and how advanced it is likely to be.
- Red blood cell count, kidney function test and liver function test are all part of the blood tests.
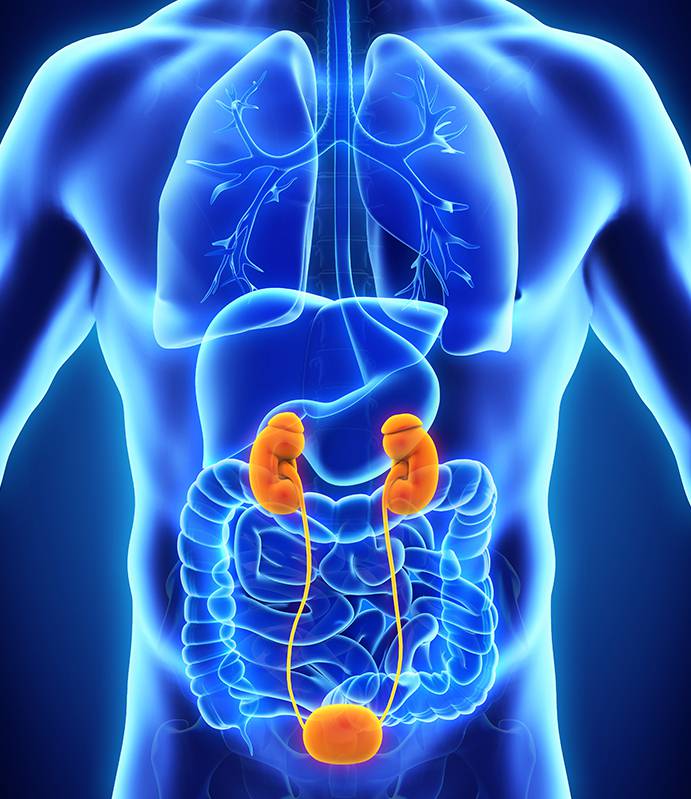
CT scan of the abdomen and pelvis:
- Testicular cancer can spread to the abdominal lymph nodes. Depending on the type of testicular cancer as determined after surgical removal and analysis of the testicle, some patients may need further surgery to remove the abdominal lymph nodes if present.
Chest X-ray or CT scan of the chest:
- To look for spread of cancer to the lungs.
MRI scan of the brain or bone scan (optional):
- To look for spread of cancer to the brain or bones if suspected.


Why is sperm banking offered to some patients?
Even though a single testicle can produce enough sperm, many patients often already have lower
sperm counts due to some underlying disorder of the testicle (e.g. undescended testis), which
predisposes them to having testicular cancer.
Subsequent treatments may be needed after surgical removal of the testicle and these interventions
can lower the sperm count (chemotherapy) or cause ejaculatory dysfunction (major abdominal surgery
- see below). Sperm banking is especially important in men who have not had children.
How is testicular cancer treated?
Testicular cancer surgery
All patients should undergo surgical removal of the testicle (radical orchidectomy) as the first step.
Surgery is done through a groin incision from which the testicle and the spermatic cord are delivered out
of the body and surgically removed. The testicle specimen can then be analysed to find out what type of
cancer it is. There are a few subtypes of testicular cancer, some of which can behave more aggressively.
Therefore, some patients may need further treatment after the surgery.
After Radical Orchidectomy
Careful observation (surveillance)
After removal of the testicle, some patients may be suitable for surveillance with regular scans, blood
tests and physical examinations, especially if the cancer is still in the early stages. This is because
some early cancers may never recur and the patient will not have to put up with treatment side effects of
radiotherapy or chemotherapy. Strict compliance and intensive follow up are required. Patients may also
have more psychological stress, worrying about possible recurrence.
Chemotherapy
Some subtypes of cancer may respond to chemotherapy. In advanced cancers, chemotherapy is usually the main treatment option. This is coordinated by a medical oncologist (doctor who specialises in cancer treatment). Different combinations and doses of chemotherapy drugs are catered individually to the patient. Side effects include nausea, fatigue, suppression of the immune system, infertility, small risk of secondary cancer, hair loss, lung complications, hearing damage and kidney damage.
Radiotherapy
Some subtypes of testicular cancer can respond to radiotherapy. Side effects include nausea, vomiting, fatigue, skin irritation, bone marrow suppression and long-term increased risks of heart disease and secondary cancer. A radiation oncologist (cancer specialist who arranges radiotherapy) supervises these treatments.
Retroperitoneal lymph node dissection
Some patients with spread of cancer to the abdominal lymph nodes may need to have them surgically removed (retroperitoneal lymph node dissection). This is a major surgery done through a large midline abdominal incision and is invasive. Side effects and possible complications include bleeding, bowel obstruction, ejaculatory dysfunction and injury to abdominal organs.
What is the prognosis?
With effective treatment options available nowadays, testicular cancer is very much a treatable condition in most patients. The prognosis depends on the subtype of testicular cancer and how advanced it is on presentation. The 5-year survival for early and moderate stage cancers are >95%.